Parkinson’s disease (PD) has been traditionally defined by the motor symptoms of bradykinesia, resting tremor, rigidity and postural instability;1 however, more recently, it has been recognized that neuropsychiatric symptoms such as psychosis, anxiety, depression, apathy, impulse control disorders and dementia are also often present in PD and can significantly impact quality of life of patients with PD.2 The American Academy of Neurology (AAN) quality improvement guidelines recommend that neuropsychiatric symptoms should be assessed annually in all patients with PD.3 When neuropsychiatric symptoms are observed, it is important to attempt to uncover the cause of these symptoms as they may be situational, medication related, the result of other medical conditions, intrinsic to PD or a combination of these factors.
The recognition and treatment of PD psychosis (PDP) is a significant unmet need. It has been estimated that over 50% of patients with PD develop psychosis at some point during their disease course.4 However, this estimate may be low as many patients do not realize that these symptoms are associated with PD or they may be hesitant to report these symptoms,5 and often physicians do not ask the patients about psychosis. In addition, reported studies have used inconsistent methodologies, assessment tools, and definitions of psychosis.6
Visual hallucinations are the most common symptom in PDP with prevalence rates increasing throughout the disease course. When accounting for dementia there is a five-fold increase in prevalence of PDP over time compared with non-demented patients.7 Less frequently, patients with PDP experience auditory, tactile and somatic hallucinations.7 The development of PDP often begins with vivid dreams and nightmares. This can be followed by the development of illusions in which a person misinterprets an existing object, such as seeing insects in a carpet pattern; presence hallucinations in which there is a feeling that someone is in the room; and passage hallucinations where a shadow, person or animal is seen briefly passing in the periphery.6,7 Initially, visual hallucinations often involve nonthreatening people or animals; however, they can still be disruptive to patients and family members and should not be ignored or go untreated. As the disease progresses, the patient often loses insight and may develop more disturbing hallucinations as well as paranoia and delusions.7–9 Risk factors for PDP include cognitive impairment/ dementia, older age, older age at diagnosis, longer disease duration, higher dosages of dopaminergic medications, more severe motor symptoms, sleep disorders, ocular disorders, and depression.5
In addition to having a significant impact on the patients’ quality of life,10 PDP significantly increases caregiver burden11 and mortality.12 PDP is also one of the strongest predictors of longterm care placement.13,14 It was shown in one study that patients with PDP placed in long-term care facilities tend to stay there permanently and have a greater mortality rate when compared to patients with PD without psychosis and older individuals in long-term care facilities from the general population.15 Additional analyses examining all aspects of care demonstrated that annual costs for PDP were $67,251 compared to patients with PD without psychosis which were $38,742.16 These data highlight the importance of early recognition of PDP and the need for effective treatment.
Treatment of Parkinson’s disease psychosis
Screening tools for PDP have been evaluated by the AAN,17 the Movement Disorder Society,18 and a more recent review evaluating the literature through 201519 and each concluded that there are no currently available scales to accurately screen for PDP and each recommended that it should be a priority to develop a PD-specific psychosis scale. Therefore, during the clinical examination, healthcare professionals should routinely ask the patient and caregiver about PDP symptoms to reduce the impact of undetected PDP. When PDP is detected, initial practices should include assurance of healthy sleep-wake cycles and good sleep hygiene. Assuring normal sensory input levels such as assessing hearing or vision deficits and applying appropriate aids if needed can also be helpful. Finally, it should be confirmed that appropriate lighting is available, and if applicable, a familiar and comfortable environment should be maintained.8 Medical conditions such as infection and dehydration can lead to psychotic symptoms and therefore, these must be considered as potential contributors and, if present, should be treated.20
PDP is thought to be a result of intrinsic factors related to PD, but can also be caused or enhanced by various medications.6 Therefore, all psychoactive non-PD medications, including anti-depressants, anticholinergics, benzodiazepines, opioids and anticholinergics should be reviewed and when possible, these agents should be reduced or discontinued.21 Once non-PD medications are at a minimum, PD medications may need to be reduced, although this may result in reduced motor function. Typically, PD medications would be slowly reduced or eliminated in the following

order: anticholinergics, amantadine, monoamineoxidase type-B inhibitors, dopamine agonists, catechol-O-methyltransferase inhibitors, and finally, levodopa.8 In consultation with the patient and caregiver, a risk/benefit based decision should be made to determine if PD medications can be reduced safely or if this should be avoided to preserve motor function and an antipsychotic medication added to the current medications.
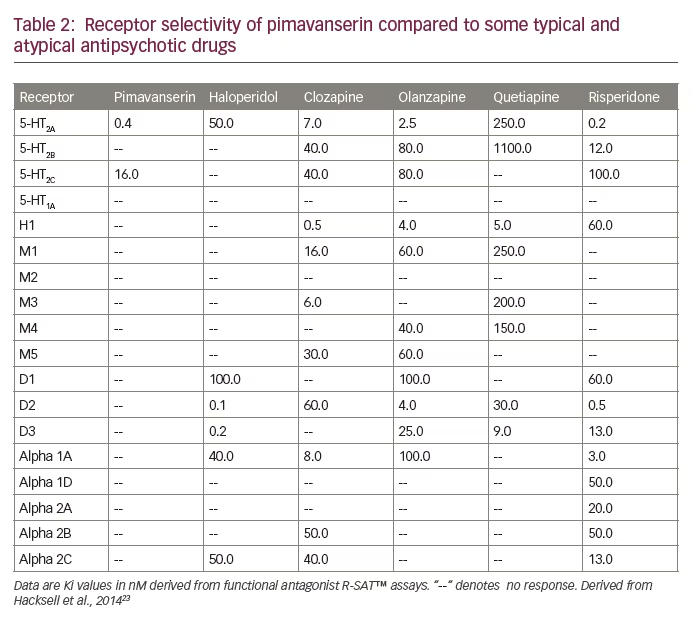
If antipsychotic medication is considered, the aim is to reduce the frequency and severity of psychotic symptoms without worsening motor function. It has been shown that treating PDP early, when symptoms are mild, is associated with better outcomes. In one study of patients with mild hallucinations with insight, deterioration to more severe hallucinations without insight occurred after 39 months in patients that were given antipsychotic medications compared to 12 months in those that did not receive antipsychotic medication.22 However, treating PDP is challenging as typical antipsychotics should not be used and atypical antipsychotics should be used with caution as they block dopamine receptors and consequently can worsen PD motor symptoms (Table 1 and Table 2).23 Furthermore, the FDA has issued a black box warning for the use of antipsychotics in elderly patients, particularly those with dementia, due to increased risk of morbidity and mortality [package inserts]. To date, there is no medication that is approved by the FDA for treatment of PDP, therefore all current medications used for PDP are used off label.
Antipsychotic treatments to avoid
Typical antipsychotics such as haloperidol, should not be used in PDP due to worsening of PD symptoms.24 The majority of the atypical antipsychotics also worsen PD motor symptoms and are not recommended for use in PDP. Small open-label reports have shown some benefit of aripiprazole for some patients with PDP; however, due to clear worsening of motor symptoms it is not recommended.25–27 Three double-blind, placebo-controlled studies showed no benefit of olanzapine compared to placebo for PDP and significant worsening of PD motor symptoms was observed.28–30 Risperidone has also been studied as a treatment for PDP. Several small open-label studies demonstrated improvement in PDP with risperidone, but results were inconsistent regarding the worsening of motor symptoms.31–34 However, in a double-blind study in which risperidone was compared to clozapine, there was improvement in PDP with both treatments, but motor symptoms were worsened more with risperidone.35 In a single-blind, open-label study, ziprasidone was shown to improve PDP without worsening PD symptoms;36 however, due to prolonged QT interval it has limited use and is not recommended for use in PDP.37
Treatment options for Parkinson’s disease psychosis
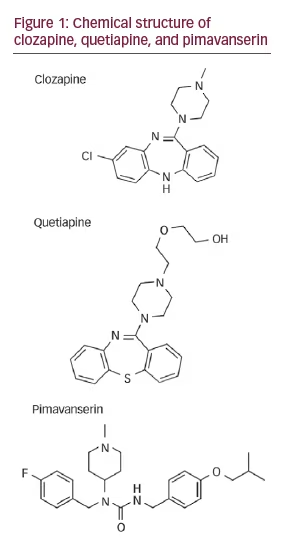
Clozapine Clozapine was the first atypical antipsychotic approved by the FDA. It is a serotonin antagonist with high affinity to the 5-HT2A/2C receptors as well as several dopamine receptors, but is a weak D2 antagonist, which reduces the likelihood of worsening PD motor function (Figure 1 and Table 2). Double-blind, controlled trials have consistently demonstrated that clozapine, at dosages from 6.25 to 50 mg/day, improves PDP without worsening PD motor symptoms.38–40 It should be noted that effective dosages for PDP are significantly lower than those used in the
treatment of schizophrenia which are typically 300-900 mg/day. Clozapine has a minimal risk of agranulocytosis which can be fatal; therefore, specialized monitoring is required consisting of weekly blood draws for the first six months, followed by every other week for the next six months and then monthly for the duration of treatment. Due to the potential side effects and specialized monitoring required with the use of clozapine, physicians often tend to avoid its use.20,41 The ability of the patient with PDP to get to the physician’s office for weekly monitoring is also a limiting factor. Other side effects of clozapine can include sedation, orthostatic hypotension, drooling and lightheadedness.
Quetiapine
Quetiapine is an atypical antipsychotic, structurally similar to clozapine (Figure 1), that also has stronger serotonergic affinity to 5-HT2 receptors than to dopamine D2 receptors (Table 2). Double-blind, placebo-controlled trials have shown inconsistent results for the efficacy of quetiapine for the treatment of PDP, although it was typically not shown to worsen PD motor symptoms.40,42–45 For PDP, quetiapine is generally started at 12.5 mg at night and increased by
the same amount every 4–7 days as needed to a maximum dosage of 300 mg/day. This dose is also lower than that used to treat schizophrenia which is typically 400–800 mg/day. It is available in both an immediate and long-acting formulation. The most common side effects include sedation and orthostatic hypotension.
Pimavanserin
In PD, the binding of 5-HT2A receptors is increased in the neocortex and it is thought that visual hallucinations are associated with an increased number of 5-HT2A receptors in the areas responsible for visual processing.46 Furthermore, in autopsies of patients with PD there are abnormalities in 5-HT receptors and increased serotonin binding in the inferior temporal cortex of patients who experience psychosis compared to those who had no psychotic symptoms.47 Pimavanserin (ACP-103; pimavanserin tartrate), which is currently under review with the FDA, is a unique drug that acts as an inverse agonist of the 5-HT2A receptors, with selectivity over 5-HT2c receptors that avoids the dopamine blockade and is therefore a promising candidate for treating PDP without worsening PD motor symptoms.48,49
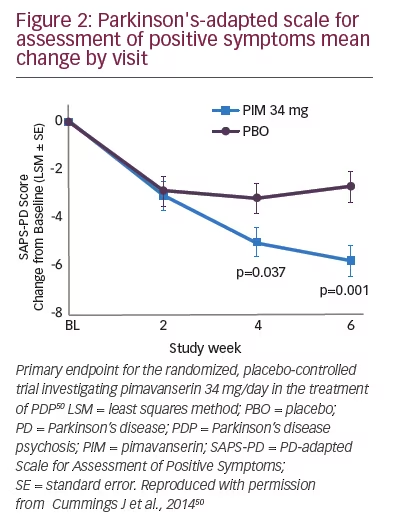
In a six-week, double-blind, placebo-controlled study [NCT01174004], the safety and efficacy of pimavanserin was evaluated in PDP patients with moderate to severe psychosis according to the Neuropsychiatric Inventory (NPI).50 The study enrolled 199 patients with PDP that had psychotic symptoms at least weekly for one month prior to screening that were severe enough to require treatment. Patients were randomized in a 1:1 ratio to either pimavanserin (34 mg) or matching placebo. The groups were well matched at baseline with the average age of both groups being 72 years, average duration of psychosis was 36 months for placebo and 31 months for pimavanserin, and average Mini Mental State Examination scores were 26.6 for placebo and 26.0 for pimavanserin, both ranging from 21–30. Unified Parkinson’s Disease Rating Scale (UPDRS) activities of daily living scores were 19 for both groups and UPDRS motor scores were 33 for both groups, indicating moderate to severe PD. Assessments occurred at baseline, 15 days, 29 days and 43 days. The primary outcome was the PD adapted Scale For Assessment of Positive Symptoms (SAPS-PD)51 from the hallucination and delusion subdomains of the SAPS. The SAPSPD includes items that occur most frequently and are sensitive to change in patients with PDP. It includes nine items, seven assessing the most frequently occurring symptoms and the global hallucination and global delusion items. There was a significant improvement in the SAPSPD demonstrating a 37% improvement with pimavanserin compared to a 14% improvement with placebo (Figure 2). It should be noted that significant changes between pimavanserin and placebo did not occur immediately, as there was no difference in SAPS-PD scores between the two groups at 15 days but significant differences were seen at both 29 and 43 days, suggesting that physicians and patients will need to be instructed that improvement may not be immediate and will occur over time. The pimavanserin group also had significant improvements in the clinician global impression of improvement and severity, caregiver burden, nighttime sleep, and daytime wakefulness. There was no worsening of PD motor symptoms in either group as measured by the UPDRS. The most common adverse events were urinary tract infection (placebo 12%, pimavanserin 13%), fall (placebo 9%, pimavanserin 11%), peripheral edema (placebo 3%, pimavanserin 7%), hallucinations (placebo 4%, pimavanserin 7%), nausea (6% both groups), and confusion (3% placebo, 6% pimavanserin), suggesting an adverse event profile comparable to placebo. Therefore, the results of this study indicate that pimavanserin is a safe and effective treatment for PDP and does not worsen PD motor symptoms.
Mortality and adverse events in PDP patients taking 34 mg of pimavanserin alone (n=357) or in combination with an atypical antipsychotic (primarily quetiapine; 79%) (n=66) as part of an open-label extension study were examined to determine the long-term safety of pimavanserin.52 The median follow-up of patients taking only pimavanserin was 421 days compared to 172 days for the combination group. Patients in the combination group had significantly more serious adverse events. In addition, the combination group had a significantly greater incidence of cognitive issues, infections and edema. Although not significant, there was also an increase in
cerebrovascular events, thromboembolic events, orthostatic hypotension and sedation in the combination group. Motor function was worsened to a significantly greater degree in the combination group as measured by the UPDRS. The mortality rate for the combination group was 18.8 deaths per 100 person-years which was significantly increased compared to 4.5 deaths per 100 person-years in the group taking pimavanserin alone. Therefore, the results of this study suggest that atypical antipsychotics should be used with caution as patients taking these drugs have an increased risk of mortality, serious adverse events, cognitive issues, edema, infections and worsening of PD motor symptoms.
Other pharmacologic approaches
Cholinesterase inhibitors, including donepezil53–55 and rivastigmine,56 have been shown to improve symptoms of PDP in case reports and small openlabel studies; however, larger controlled studies are necessary to determine if these agents may be beneficial for PDP. A case report has suggested a potential benefit of mirtazapine for PDP;57 however, antidepressants have been shown to induce or exacerbate psychotic symptoms,58–59 so further research is necessary to determine if this is a reasonable treatment option for PDP. Finally, in a small, open-label study, the 5-HT3 receptor antagonist, ondansetron, was shown to provide moderate to marked improvement in PDP without worsening PD motor symptoms.60 Further research would be needed to replicate these findings in larger, controlled trials.
Summary
Patients with PD frequently experience psychosis which negatively impacts patient quality of life, caregiver burden and healthcare expenditures. At this time, there is no FDA approved treatment for PDP. Initial management of PDP includes evaluation for medical conditions such as dehydration or infection, reducing or withdrawing potentially offending non-PD medications, and reducing or discontinuing PD medications if possible without worsening PD symptoms. If PDP symptoms do not improve a PDP treatment should be considered. Typical antipsychotics should not be used for PDP due to worsening of PD motor symptoms and the majority of atypical antipsychotics also have the potential to worsen PD symptoms. Currently, clozapine and quetiapine have had the most success in reducing psychotic symptoms without worsening PD and quetiapine is the most commonly prescribed medication for PD psychosis as it does not require routine blood monitoring. The development of pimavanserin, a selective serotonin 5-HT2A inverse agonist without D2 dopaminergic affinity represents an important advance in PDP treatment. With its receptor selectivity, pimavanserin is able to provide antipsychotic benefit without the adverse effects associated with typical and atypical antipsychotics.